Our Services
Reduce Your Stress While Increasing Efficiency

Eligibility Check
We prevent claim denials by confirming patient’s coverage from the insurance before claim submission.
Claim Submission
We submit claims using your EMR software to avoid disruption of your operations or having to retrain your staff. Our team is well versed with a large number of EMRs. We check clearinghouses for rejections within 24-hrs and follow up.
Denial Management
We immediately investigate and appeal denied claims to maximize your reimbursements. We also analyze denials to identify common reasons (e.g., specific procedures, ICD’s, documentation, etc.) and suggest corrective actions to reduce recurrence of preventable denials.

Payment Posting
We promptly post payments received from patients & insurance via ERA/EOB and reconcile data to identify any discrepancies.
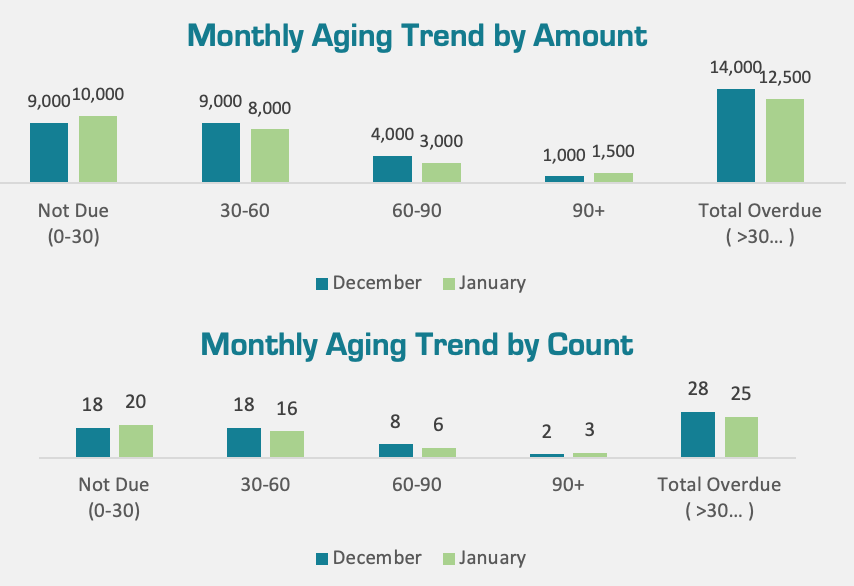
Accounts Receivable
We do aggressive follow up on your outstanding claims & patient dues for prompt payments. We generate and analyze aging reports to identify and prioritize overdue accounts for a systematic follow up.
Reporting and Analytics
We go beyond claims management to help your practice succeed. Our team provides an in-depth reporting and analysis of your billing, offering both daily and monthly reports based on mutually agreed Key Performance Indicators (KPIs).
Add-On Services
- Credentialing (initial and ongoing)
- Patient In-take
- Patient follow-up and appointment reminders
- Social media management
Let us transform your billing into an efficient, stress-free process.
Contact Us
© 2024 All Rights Reserved.
